Research article/ Open Access
DOI:10.31488/EJRM.142
Effects of Physical Therapy Intervention in Pneumonia Patients According to the Severity of Illness
Yusuke CHIGIRA*1 PT, PhD, Yoichi OHNO1 PT, PhD, Nobuyuki TAKEUCHI1 PT, PhD, Kunio DOBASHI2 PhD
1. Department of Physical Therapy, Faculty of Health Science, Takasaki University of Health and Welfare, Japan
2. Jobu Hospital for Respiratory Diseases, Japan
*Corresponding author: : Yusuke CHIGIRA, Department of Physical Therapy, Faculty of Health Science, Takasaki University of Health and Welfare: 501 Nakaoorui, Takasaki, Gunma 370-0033, Japan, Tel: +81 27-352-1291
Abstract
Purpose: The effects of physical therapy on elderly patients admitted to the ICU due to pneumonia were evaluated according to the severity of illness. Methods: Intervention by physical therapists was initiated in the super-acute phase on the day after admission. The patients were divided into groups I, II, and III according to the level of severity. The duration of stay in ICU, duration of hospitalization, and ADL before and after admission were evaluated. Results: Overall, the duration of stay in the ICU and duration of hospitalization were longer, and changes in total functional independence measure (FIM) score were larger, but ADL at discharge was poorer, as the condition was severer. Concerning the effects of intervention according to severity, significant improvements were observed in the values of motor function, cognitive function, and total FIM score in all groups. Conclusions: The effects of physical therapy in elderly pneumonia patients admitted to the ICU were evaluated according to the severity. In group I at the lowest severity level, changes were not large probably because of the low severity of the illness, shortness of the duration of stay in the ICU, and mild progression of disuse syndrome. Improvements were observed in the values of motor function, cognitive function, and total FIM score in all groups, and physical therapy early after the onset of pneumonia was confirmed to be effective.
Key words: Elderly pneumonia patients, early physical therapy, CURB-65, functional independence measure (FIM)
Introduction
Since the mortality due to pneumonia in people aged 65 years and over is very high, being 95% or higher, in Japan, [1] it is important to improve the care of pneumonia patients in the acute phase, and early intervention by physical therapists is recommended.
Early resumption of ambulation is known to exert favorable effects on respiratory, circulatory, motor, and psychological aspects of patients, but many pneumonia patients are forced to stay in bed for a long time due to excessive emphasis on rest during treatment and suffer decreases in activities of daily living (ADL).
Physical therapy in the ICU causes very few adverse events and can be performed safely with sufficient risk management [2]. Many studies have been conducted on the effects of exercise therapy early after admission to the ICU and early resumption of ambulation, [3] leading to increased awareness of the risk of impairment of functions and ADL associated with prolonged stay in the ICU [4]. Early initiation of rehabilitation primarily by physical therapists is an important intervention for preventing disuse syndrome due to pneumonia and securing of ADL after discharge.
We, therefore, initiated physical therapy in elderly pneumonia patients early after admission to the ICU, and evaluated its effects on the duration of stay in the ICU, duration of hospitalization, and ADL at discharge by the severity of illness.
Methods
Patients
The subjects were patients admitted to the ICU due to community-acquired pneumonia. The patients who presented with radiographic evidence and clinical symptoms of pneumonia and fulfilled the criteria of the revised American Thoracic Society score (rATS) [5] for admission of pneumonia patients to the ICU were treated in the ICU.
Early physical therapy was initiated on the day after admission due to pneumonia in 82 patients, and they were divided according to the severity at the time of admission into groups I, II, and III with CURB-65 scores of 3, 4, and 5, respectively [6]. Patients who were bed-ridden before the onset of pneumonia, and those with serious complications such as severe heart failure, were excluded (Figure 1). This study was carried out with approval by the institutional review board of Kan-etshu-chuo-Hospital (approval No.: 201306051) and with sufficient consideration of protection of the subjects’ personal information based on the Declaration of Helsinki.
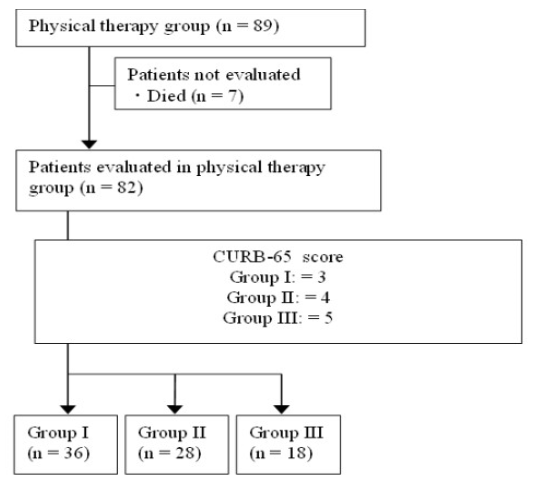
Figure 1:Flow diagram of the patients
Intervention methods
Intervention by physical therapy consisted of guidance in respiration practice, assistance in expectoration of sputum, upper limb/lower limb range of motion exercise (ROM ex) initiated on the day of, or the day after, admission, aiming at the earliest possible resumption of ambulation.
In respiration practice, the patients were instructed with assistance to take 10 slow and deep breaths from immediately after admission [7]. Also, the patients practiced self-sputum expectoration by the active cycle of breathing technique with assistance until they became able to do it independently [8].
ROM ex was performed in the shoulder girdle, shoulder, elbow, wrist, and fingers in the upper limb and in the hip, knee, ankle, and toes in the lower limb in all directions and ranges of motion. It was performed from the day of admission even if the patient was unconscious and could not follow instructions. ROM ex was started with passive exercise and advanced to active exercise as the patient became able to follow instructions.
Ambulation was resumed on the day of admission if the temperature was controlled at 38C or below. It was discontinued if a fever of 38C or above, orthostatic hypotension, vomiting, or respiratory distress was observed. Ambulation was started from the seated position in a wheelchair and advanced to standing up and walking according to the patient’s condition. Intervention was performed for about 40 minutes once a day in all severity groups.
Evaluation items
The evaluation items were sex, age, BMI, duration of stay in the ICU, duration of hospitalization, and Functional Independence Measure (FIM) [9] scores before admission and at discharge. The severity was evaluated using CURB-65 [6]. The score of CURB-65 is calculated from the data of four tests and age. It ranges from 0 to 5, with 5 indicating the greatest severity.
ADL was evaluated using FIM,9) and the scores before admission and at discharge were examined. The FIM scores before admission and at discharge were evaluated as FIM changes. The FIM scores before admission were based on information obtained by interviewing the patients and their families.
Statistical Analyses
The background and FIM changes were compared according to severity using the Kruskal-Wallis test, followed by multiple comparisons using Wilcoxon’s signed rank sum test with Bonferroni’s modification of inequality. The effect of intervention was compared according to severity using Mann-Whitney’s U-test.
Statistical analyses were performed using SPSS statistics (version 17.0, IBM, USA) at the 5% level of significance.
Results
Generally, the duration of stay in the ICU and the duration of hospitalization were longer, and the changes in total FIM score (Table 1) were greater, but ADL at discharge was poorer, as the condition was severer.
Table 1.All pneumonia patients
| Number of subjects | 82 |
|---|---|
| (male/female) | (54/28) |
| Age (years) | 81.44±7.52 |
| BMI | 20.25±2.3 |
| Number of patients mechanically ventilated on admission (persons) | 16 |
| Duration of stay in the ICU (days) | 10.93±3.76 |
| Duration of hospitalization (days) | 30.44±15.9 |
| FIM score before admission | 82.16±9.47 |
| Motor function | 57.61±7.89 |
| Cognitive function | 24.55±2.56 |
| FIM score at discharge | 66.65±12.45 |
| Motor function | 45.91±10.19 |
| Cognitive function | 19.54±3.57 |
| FIM change | 15.41±6.69 |
| Changes in motor function | 11.70±5.46 |
| Changes in cognitive function | 5.01±2.25 |
| Mean±SD *: p < 0.05, **: p <0.01 | |
| BMI: Body-mass index | |
| FIM: Functional independence measure | |
Concerning the effects of intervention according to severity, significant improvements were observed in motor function, cognitive function, and total FIM score in groups I, II, and III (Table 2).
Table 2.Background and changes in FIM score according to severity
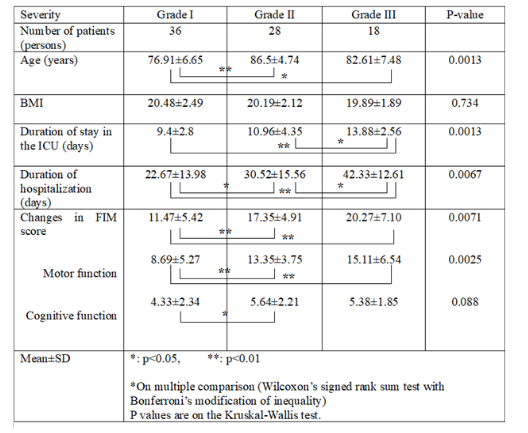
Table 3.Effects of intervention according to severity
| Severity | Grade I | Grade II | Grade III | |||
|---|---|---|---|---|---|---|
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | |
| Total FIM score | 85.97±9.30 | 74.28±10.05** | 80.46±8.09 | 63.11±9.74** | 77.17±9.14 | 56.89±11.71** |
| Motor function | 59.97±7.41 | 51.28±8.42** | 56.96±7.09 | 43.61±8.42** | 53.89±8.75 | 38.78±10.63** |
| Cognitive function | 25.61±2.67 | 21.67±3.35** | 23.50±1.66 | 17.86±2.81** | 23.28±2.05 | 17.89±2.82** |
| Mean±SD**: p<0.01 | ||||||
Discussion
Physical therapy was performed in elderly pneumonia patients admitted to the ICU, and its effects were evaluated according to the severity of illness. Changes were not large in group I with the lowest severity level. This was probably due to the mildness of the illness, shortness of the duration of stay in the ICU, and low grade of disuse syndrome.
BMI was reported to show the highest accuracy in predicting 1-year mortality, and may be useful for the identification of patients with a poor long-term prognosis, [10] but, in this study, no significant difference was observed in BMI among the groups.
Improvements were observed in motor function, cognitive function, and total FIM score in groups I, II, and III, and early physical therapy after the onset of pneumonia was suggested to be effective.
Concerning motor function, prevention of intensive care acquired weakness (ICUAW) is important.
Lack of activity is considered to be a factor of ICUAW and is reported to be related to prolongation of the duration of the use of mechanical ventilation and stay in the ICU and delay of recovery of ADL [11]. In this study, intervention was made by minimizing the inactive period.
As it was reported that the number of steps per day after recovery decreases with the degree of severity [12], the effect of ICUAW may be considerable. Proactive prevention of the loss of muscle mass is likely to contribute to recovery of elderly pneumonia patients, [13] and continuation of passive joint range of motion exercise even if the patient was unconscious and did not respond to instructions is considered to have exerted favorable effects on motor function.
Hopkins et al. reported no relationship between impairment of cognitive function after intensive care and the severity of acute respiratory distress syndrome, or duration of stay in the ICU [14]. In this study, however, the duration of hospitalization and stay in the ICU was longer, and the decline in cognitive function increased with the severity of illness. Shortening of the duration of stay in the ICU by physical therapy intervention may alleviate the decline in cognitive function.
Many critically ill patients admitted to the ICU reportedly show a decline in the cognitive level due to delirium [15]. However, delirium was reduced by physical therapy in patients with acute respiratory impairment and mechanically ventilated patients, [16,17] and intervention with physical therapy is also important for critically ill patients.
It has been reported that a high percentage of elderly patients died or exhibit functional declines from 30-day hospitalization due to pneumonia regardless of the severity of illness [18]. In this study, the mean duration of hospitalization exceeded 30 days in groups II and III. In addition, there is a report that, in pneumonia patients, the severer the illness, the higher the cost of inpatient care [19].
Further evaluation is considered necessary for accelerating the relief of symptoms and shortening of the duration of hospitalization by early intervention with physical therapy.
Conclusions
Intervention with physical therapy for pneumonia patients in the ICU may be effective regardless of the medical conditions, despite differences in effects according to the severity. Since physical therapy is expected to contribute to the prevention of complications and maintenance/improvement in ADL, further evaluation is necessary.
Acknowledgements
We thank intensive care team members for participation as physical therapists and nursing team for their substantial collaboration.
Conflict of Interest
Authors have no conflict of interests to disclose. The data analyzed in this study were obtained in 2017-2019 before SARS-CoV-2. This manuscript is not under consideration for publication elsewhere.
References
1. Teramoto S, Fukuchi Y, Sasaki H, et al. High incidence of aspiration pneumonia in community – and hospital – acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc. 2008; 56: 577-579.
2. Schweickert WD, Kress JP. Implementing early mobilization intervention in mechanically ventilated patients in the ICU. Chest. 2011; 140: 1612-1617.
3. Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: A quality improvement project. Arch Phys Med Rehabil. 2010; 92: 536-542.
4. Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011; 344: 1298-1304.
5. Phua J, Ngerng WJ, Lim TK. The impact of a delay in intensive care unit admission for community-acquired pneumonia. Eur Respir J. 2010; 36: 826-833.
6. Lim WS, van der Eerden MM, Laing R, et al. Macfarlane JT. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003; 58: 377-382.
7. Pasquina P, Tramer MR, Granier JM, et al. Respiratory physiotherapy to prevent pulmonary complications after abdominal surgery. Chest. 2006; 291: 1753-1762.
8. Cecins NM, Jenkins SC, Pengelley J, Ryan G. The active cycle of breathing techniques-to tip or not to tip? Respir Med. 1999; 93: 660-665.
9. Keith RA, Granger CV, Hamilton BB, et al. The functional independence Measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987; 1: 6-18.
10. Astrid Malézieux-Picard, Leire Azurmendi, Sabrina Pagano, et al. Role of Clinical Characteristics and Biomarkers at Admission to Predict One-Year Mortality in Elderly Patients with Pneumonia. J Clin Med. 2021; 25: 105.
11. Kress JP, Pohlman AS, O`Connor MF, et al. Daily Interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl Med. 2000; 342: 1471-1477.
12. Hayley Rice, Kylie Hill, Robin Fowler, et al. Reduced Step Count and Clinical Frailty in Hospitalized Adults With Community-Acquired Pneumonia. Respir Care. 2020; 65(4): 455-463.
13. Keisuke Maeda , Junji Akagi, et al. Muscle Mass Loss Is a Potential Predictor of 90-Day Mortality in Older Adults with Aspiration Pneumonia. J Am Geriatr Soc. 2017; 65: 18-22.
14. Hopkins RO, Weaver LK, Collingridge D, et al. Two-year cognitive, emotional, and quality-of-life outcome in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005; 171: 340-347.
15. Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004; 291: 1753-1762.
16. Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009; 373: 1874-1882.
17. Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: A quality improvement project. Arch Phys Med Rehabil. 2010; 92: 536-542.
18. Chan Mi Park, Wonsock Kim, Hye Chang Rhim, et al. Frailty and hospitalization-associated disability after pneumonia: A prospective cohort study. BMC Geriatr. 2021; 5: 111.
19. Ayça Gümüş, Aykut Çilli, Özlem Çakın, et al. Factors Affecting Cost of Patients with Severe Community-Acquired Pneumonia in Intensive Care Unit. Turk Thorac J. 2019; 30; 216-223.
Received:December 20, 2023;
Accepted: January 11, 2024;
Published: January 16, 2024.
To cite this article : Chigira Y, Ohno Y, Takeuchi N, Kunio Dobashi K. Effects of Physical Therapy Intervention in Pneumonia Patients According to the Severity of Illness. European Journal of Respiratory Medicine. 2024; 6(1): 398 - 402. doi: 10.31488/EJRM.142.
© The Author(s) 2024
