Case Report / Open Access
DOI: 2021; 3(1): 163 - 166. doi: 10.31488/ejrm.111
Inspiratory Muscle Training with an Electronic Device to Facilitate Weaning Ventilatory of a Patient with COVID-19
Leonardo Cordeiro de Souza*1,2, Amarildo Abreu de Souza2, Fernando da Franca Oliveira2
1. Faculdade de Fisioterapia, Universidade Estácio de Sá, Niterói – RJ, Brazil
2. Unidade de terapia Intensiva, Hospital e Clínica São Gonçalo, São Gonçalo - RJ, Brazil
*Corresponding author: Leonardo Cordeiro de Souza, Gestor de fisioterapia do Hospital Icaraí and Hospital e Clínica São Gonçalo, Rua Marquês de Paraná, 233 – 5o. Andar, CEP 24030-215 - Centro, Niterói – RJ, Brasil.
Abstract
In December 2019 in China, a new coronavirus (COVID-19) spread globally reaching many countries being declared a pandemic state, in which the severe form of the disease results in respiratory failure requiring mechanical ventilation (MV). In this scenario, many patients remained in MV for several weeks due to severity and secondary complications, such as respiratory and systemic muscle weakness, resulting in prolonged weaning, a condition that alone is related to a high mortality rate. The study is reporting a case of a patient with COVID-19 who underwent an inspiratory muscle-training (IMT) program to facilitate prolonged weaning after 29 days of controlled ventilation. The patient was successful after 9 days of IMT and the hospital discharged from the hospital after 66 days.
Keywords: mechanical ventilation; weaning; maximum inspiratory pressure; Training inspiratory muscle
Introduction
In December 2019 in China, a new coronavirus (COVID-19) spread globally reaching many countries being declared a pandemic state [1]. The severe form of the disease results in respiratory failure requiring mechanical ventilation (MV), use of sedation, and neuromuscular blocker for several weeks [2,3]. The previous report demonstrated that the diaphragmatic dysfunction induced by MV and polyneuropathy acquired in the ICU, which results in prolonged weaning, a condition which itself is related to a high mortality rate [4].
Inspiratory muscle training (IMT) with resistive load can be the main expectation of current therapy in the search for ventilator independence [5-7]. The 2015 meta-analysis and the recent study by Guimarães and cols, points out that the use of IMT considerably increases the success rate of weaning extended 8,9. In addition, Inspiratory muscle strength can be evaluated and guided by serial measurements timed inspiratory effort index, reported as a useful tool to aid ventilation weaning [6,7,9,11].
This is a report of a case of respiratory muscle weakness acquired in ventilation mechanical that has undergone an IMT program with an electronic load visually oriented by the computer screen.
Methods
A case report of a patient who remained in the intensive care unit of a hospital in the state of Rio de Janeiro, Brazil, from April 26 to June 2, 2020, in which was obtained a free and informed consent form.
Procedures
A timed inspiratory effort index (TIE) was calculated as the ratio of the PImax recorded after the first 30 seconds of observation by the corresponding time to reach it, keeping occluded airways with a one-way valve for up to 60 seconds [9-11].
For the measurement of maximal inspiratory pressure (PImax) and the TIE index, were used the digital vacuometer and MagnaTIE (Magnamed, São Paulo, SP, Brazil), with a scale of 300 cmH2O and 0.1 cmH2O increments and time interval of 100ms for each Pressure.
As a safety measure during the use of the TIE index, the study subject was kept under surveillance, through the multi parameter monitor to which the perception of some sign of instability by the examiner the test should be interrupted and the patient returned to MV [9-11].
The patient was positioned to 45 degrees. The cuff of the orotracheal tube was hyperinflated to prevent leaks during measurement. After tracheal aspiration, the patient remains connected to the mechanical ventilator for two minutes with 100% oxygen-inspired fraction (FIO2) [9-11].
After hyperoxygenation, the mechanical ventilator was disconnected and, after 10 seconds of spontaneous breathing, the digital vacuometer was manually connected at the end of exhalation the artificial airway, keeping it occluded for up to 60 seconds, in which it is recorded the values corresponding to each inspiratory effort [9-11].
Weaning success was predicted by TIE index values ≥1.0 cmH2O/s when the patient maintained spontaneous breathing uninterruptedly for 5 days. The decision to return mechanical ventilation was taken based on the low tolerance signals used routinely in the hospital [6,7,9-11].
The IMT was held daily between 08:00 and 10:00 AM. The intermittent protocol established consisted of imposing an inspiratory load for 30 respiratory cycles in three periods (Figure 1). Each period of 10 respiratory cycles was divided into two stages: in the first, the load was gradually increased until the target was reached (50% of the PImax); in a second, the remaining 5 respiratory cycles of the period were performed under the target load. At the end of the third period, the patient had a rest period (breathing without inspiratory load) of 2-3 minutes, and underwent three more periods of training totalizing 6 periods (60 breathing cycles) of training at a time. If signs of intolerance were observed during IMT the patient returned to MV. After each training session, the patient returned to MV in PSV mode for two hours to rest, and was subsequently progressive gradual withdrawal protocol with tracheal collar, with the aim of increase spontaneous breathing time daily [9,11]. The patient was reassessed weekly with the TIE index for incremental adjustment of the target load until it reaches 70% of the PImax [9,11].

Figure 1.Panel A - Software screen with protocol customization in cycles incremental and interval; Panel B - Demonstration of the connection of the equipment in the cannula tracheostomy, and visual feedback from the screen with the patient during the execution of training; Panel C - Illustration of the resource (SITcare) used in the rehabilitation program to resume the function of sitting at the bedside.
Case Report
Male, 59 years old, hypertensive and obese grade 2 (BMI=36), was admitted in the general hospital and transferred intensive care unit (ICU) on April 26, 2020, with fever (38.5 °C), tachypnea, a fall in oxygen saturation, and reported difficulty breathing. His laboratory exams data showed a predominantly peripheral frosted glass lesion (25%) compatible with the findings by the new coronavirus, laboratory data were: pH 7.43, PaO2 45 mmHg, PaCO2 39 mmHg, HCO3 25 mEq/L and SaO2 83%, Ferritin 1379 ng/mL, D-dimer 0.2 ng/dl, hemoglobin 11.0 g/dL, Leukometry 5,730 mm, Bands 1%, Lymphocytes 6%, and C-reactive protein 30.7 mg/dL. On the second day of admission, the RT-PCR test was reagent for Sars-CoV-2.
Upon arriving at the ICU, the patient began treatment with oxygen therapy with a reserve bag of 10 L/m and awake prone positioning but did not present satisfactory gasometry stability. In the morning of April 28 day, was initiated noninvasive ventilation with a full face mask coupled in the mechanical ventilator alternating between the prone and supine position, in which he still maintained the condition of type 1 acute respiratory failure. Thus, was done sedation, orotracheal intubation, and mechanical ventilation (MV) with pressure controlled ventilation mode (PCV) by the 840TM mechanical ventilator (Covidien-Nellcor and Puritan Bennett, USA). Due to the severity of his clinical condition, he was maintained in this regimen until the beginning of the weaning process, remaining on MV until May 29, 2020.
During this period of MV, He evolved with Respiratory Discomfort Syndrome (ARDS), being curarized and ventilated with the tidal volume between 6 to 8 ml/kg, high oxygen fractions (FIO2 >50%), PEEP between 12 to 16 cmH2O, and prone ventilation. Presented acute renal failure and hemodialysis was necessary, and ultimately blood cultures were positive for MRSA and VRE, in which he developed septic shock. Vasoactive amines and various antimicrobial agents were administered for several weeks.
The patient was tracheostomized after 14 days of intubation. From the twenty-first day of ventilation remained awake, cooperative, hemodynamically stable, and infection-free until it reaches successful ventilatory weaning. During unsuccessful attempts to wean, where he could not tolerance the spontaneous breathing more than 15 minutes, the inspiratory muscle-training program (IMT) was instituted on the 29th day of MV. He was using the isokinetic electronic load device (POWERbreathe K-5, London, United Kingdom), in which three sets were made with 20 repetitions to achieve the 60 efforts intermittently and incrementally, daily, until respiratory total independence, figure 1.
Were used the Medical Research Council (MRC) to assess skeletal muscle strength, and the functional status score (FSS-UTI) to assess the degree of independence. When the IMT program was started, after 29 days on MV, He MRC was 6 (10% of normal) FSS 3 (9% of normal). At that time, his PImax was 24 cmH2O (22% of normal) and the TIE index 0.27 cmH2O/s, and the training load was adjusted to 12 cmH2O (50% of PImax). On the 33rd day of MV, his PImax had increased to 47 cmH2O, with a TIE index of 0.82 cmH2O/s, and the training load was readjusted to 28 cmH2O (60% of PImax). On day 37, PImax reached 61 cmH2O, the TIE index 1.29 cmH2O/s, and the training load was reajusted again to 40 cmH2O (70% of PImax) and the patient was removed successfully of the mechanical ventilator.
Daily training was maintained until the placement of the metallic cannula on June 15th, in which the patient reached the 95 cmH2O and the TIE index 1.87 cmH2O/s (Figure 2). Discharge him from the ICU after 55 days of hospitalization. In addition to the IMT program, was accompanied by a hospital rehabilitation protocol, in which acomplished daily of the physiotherapy from the initial period of the ICU. Thus, the MRC at the end of hospitalization was 36 (60% of normal) and FSS of 19 (54% of normal). On July 2, 2020, the patient was discharged after 66 days of hospitalization.
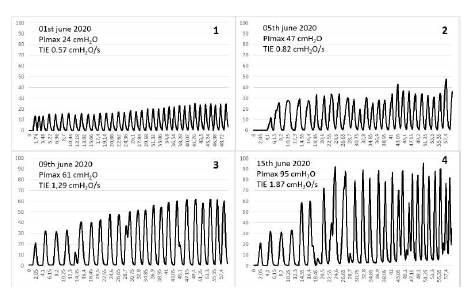
Figure 2.Graphs ((pressure, cmH2O /time, seconds) of the serial measurements of the inspiratory peaks by the TIE method of the first until the last measurement throughout the inspiratory muscle training program.
Discussion
Prolonged MV is associated with several complications, such as pneumonia associated with ventilation (VAP), ventilation-induced diaphragmatic dysfunction (DDIV), and polyneuropathy of the critical patient [3]. In a prospective, randomized and blind research, in which 312 patients on prolonged ventilation were analyzed (median permanence of 34 days on MV). The success rate of weaning was 49%, patients who returned to mechanical ventilation after weaning success, 12.1%, mortality rate 55%, and mortality after 1 year, 63% [4].
Several efforts have been made in an attempt to reduce VM time, ICU permanence time, and the immobility sequence. To this end, some studies have used the IMT with encouraging results. The use of IMT is associated with an increase in the rate of prolonged weaning success (71% compared to 47% in the control group) [5]. In a systematic review, it was clear that only patients with weaning ventilatory difficulties benefited from IMT [8]. IMT seems to emerge as an important adjuvant therapeutic tool to address the weaning of long-term patients on MV [5,8,9]. However, it is still unclear what type of protocol should be used: load, duration, intensity, and frequency. In this sense, the team's experience with cases and the use of the TIE index to diagnose respiratory muscle weakness and guide the training prescription seems to be resulting in higher success rates [6,7,9-11].
The TIE index was conceived by Souza et al. [6] and considers the combination of stimulation of the respiratory center and muscle response time. In several publications, this index showed better accuracy than the other (f/Vt, PImáx, IWI, P0.1) to predict the outcome of weaning ventilatory and guide respiratory muscle training [6,7,10]. It is understood that this new tool allows the quantitative evaluation of the inspiratory musculature, supplanting the clinical judgment to guide the prescription of parameters and assist in the process of rehabilitation.
The evaluation of the MRC before and after the hospital rehabilitation protocol had a significant improvement, in which he was initially scored at 6 (10% of normal), indicating weakness, and at hospital discharge, the score was 36 (60% of normal). Similar data was also pointed out with the FSS-ICU scale, which went from 3 (9% of normal) to 19 (54% of normal). Other reports suggest that encouraging early functionality in the ICU may reduce the duration of MV and length of stay in the ICU [6,7].
Few studies were found using the same electronic isokinetic inspiratory load device, which reported an increase in inspiratory muscle strength and results favorable for weaning [6-9]. Thus, more prospective and randomized clinical studies must be done so that conclusions on the definitive role of this new resource to facilitate prolonged weaning can be clarified. About the myopathy by Sars-Cov-2, we still are waiting for evidences.
In conclusion, the use of IMT with electronic load and visual feedback guided by the TIE index increased the gain of inspiratory muscle strength and resistance that can have resulted a successful weaning ventilator in the patient with viral pneumonia by Sars-Cov-2.
Acknowledgement
The authors would like to thank all respiratory physiotherapists and physicians in the therapy unit hospital and Clínica São Gonçalo (RJ) for their collaboration in our study.
Author’s Contributions
Leonardo C. de Souza contributed to the conception and preparation of the manuscript. Amarildo Abreu and Fernando da Franca assisted in patient care and in the writing and review of the case report.
Support
Funding for Publication and Support by Magnamed, São Paulo, Brazil. Responsible for the Magna TIE project: Toru Miyagi (Chief Engineer). POWERbreathe support, London, United Kingdom. Responsible for the donation of KH2: Harry Brar (President)
Conflicts of Interest
In the research, we received a POWERbreathe KH2 device for the treatment of patients, neither the funding agency nor any external organization participated in the design or has any competitor of interest. POWERbreathe had the final approval of the manuscript.
References
1. World Health Organization. (2020). Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected interim guidance.2020.
2. Pan L. How to face the novel coronavirus infection during the 2019–2020 epidemic: the experience of Sichuan Provincial People’s Hospital. Intensive Care Med. 2020.
3. Peñuelas O, Keough E, López-rodríguez L, et al: Ventilator-induced diaphragm dysfunction: Translational mechanisms lead to therapeutical alternatives in the critically ill. Intensive Care Med Exp. 2019; 7:1–25
4. Jubran A, Grant BJB, Duffner LA, et al. Effect of pressure support vs unassisted breathing through a tracheostomy collar on weaning duration in patients requiring prolonged mechanical ventilation. A randomized trial. JAMA. 2013; 309: 671-677.
5. Martin AD, Smith BK, Davenport P, et al. Inspiratory muscle strength training improves weaning outcome in failure to wean patients: a randomized trial. Critical Care. 2011; 15:R84.
6. Souza LC, Campos JFR, Daher LP, et al. Mechanical Ventilation Weaning in Inclusion Body Myositis: Feasibility of Isokinetic Inspiratory Muscle Training as an Adjunct Therapy. Case Rep Crit Care. 2014; 902541.
7. Souza LC, Souza AA, Almeida EEP, et al. Inspiratory muscle training with isokinetic device to help ventilatory weaning in a patient with Guillain-Barré Syndrome by Zika Virus. Case Rep Crit Care. 2018; 18:1-5
8. Mark E, Ruth D. Inspiratory muscle training facilitates weaning from mechanical ventilation among patients in the intensive care unit: a systematic review. J Physiother. 2015; 61:125-134.
9. Da Silva Guimarães BL, de Souza LC, Cordeiro HF, et al. Inspiratory Muscle Training With an Electronic Resistive Loading Device Improves Prolonged Weaning Outcomes in a Randomized Controlled Trial. Crit Care Med. 2020.
10. Souza LC, Guimarães FS, Lugon JR: Evaluation of a new index of mechanical ventilation weaning: the timed inspiratory effort. J Intensive Care Med; 2015; 30:37-43.
11. Da Silva Guimarães BL, de Souza LC, Guimarães FS, et al. Serial weekly measurements of the timed inspiratory effort index can predict successful prolonged weaning. Respir Care. 2019;64(10):1286-1292.
Received:February 03, 2021;
Accepted:February 11, 2021;
Published:February 25, 2021.
To cite this article : De Souza LC, De Souza AA, Oliveira FDF. Inspiratory Muscle Training with an Electronic Device to Facilitate Weaning Ventilatory of a Patient with COVID-19. European Journal of Respiratory Medicine. 2021; 3:1.
© 2021 De Souza LC, et.al.
