Casereport/ Open Access
DOI:10.31488/EJRM.129
The Bright Side of COVID-19 Pandemic Vis-À-Vis Neglected Diseases: Three Asylum Seeker -Patients with TB- COVID19 Co-Infections
Lian Bannon*1, Omer Shlesinger2, Fadi Kinaany2, Giris Jacob1, Jacob N Ablin2, Ronit Cohen-Poradosu3
1. Department of Internal Medicine F, Tel Aviv Sourasky Medical Center, Israel
2. Department of Internal Medicine H, Tel Aviv Sourasky Medical Center, Israel
3. Infectious Diseases Unit, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel
*Corresponding author: FLian Bannon, Department of Internal Medicine F, Tel Aviv Sourasky Medical Center, Israel.
Abstract
The novel COVID-19 pandemic may coexist with a venerable lethal infectious disease, tuberculosis (TB), which remains a leading cause of death worldwide. Data regarding the manifestations and consequences of COVID-19 /TB co-infection is scarce. Due to extra precautions taken during the pandemic, even patients lacking medical insurance presenting with/without respiratory complaints, have been referred to complete both a SARS-CoV-2 PCR test and a chest X-Ray, thus increasing the chance of detection of unsuspected TB. Herein we describe three cases of Eritrean asylum seeker patients diagnosed with TB/COVID-19 co-infection at the time of presentation to our facility. All three were young, immunocompetent, had active pulmonary or extrapulmonary TB, were negative for HIV infection, and were COVID-19 symptom free. Observing these three patient’s disease’s patterns, we assumed that the influence of active TB on COVID-19 was minor. However, the presence of COVID-19 may theoretically contribute to activation or clinical manifestation of latent/active TB.
Background
As attention of both the medical community and the general public have been focused on the overwhelming surge of the novel COVID-19 pandemic, attention has naturally been drawn away from more classic and less publicized, although not less lethal, infectious diseases such as Tuberculosis, still constituting the leading cause of morbidity and mortality among infectious diseases worldwide, causing 1.5 million deaths in 2018,[1]. In the current case report, we present three cases of co-infection with SARS-Cov-2 and TB, and attempt to demonstrate an unexpected positive spin-off of the current situation – the possibility of earlier identification and treatment of TB due to the pandemic. This development is the result of both infections primarily involving the pulmonary system,[2], thus leading to widespread chest imaging, through X-ray and /or Computed Tomography (CT) scans.
While various and sometime conflicting reports have been published regarding the co-occurrence of TB and COVID-19, ours appears to be the first report focusing on the early diagnosis of (unsuspected) TB due to COVID-19.
Case Presentation
Case number 1
A 34-year-old Eritrean - born male patient, with a history of chronic progressive low back pain, presented to the Emergency Room (ER) due to new onset weakness of the lower extremities. Upon arrival, PCR of SARS-CoV-2 was found to be positive with cycle threshold (Ct) value of 22. A Chest X - ray exam was normal. The patient was admitted to a COVID-19 isolation ward and underwent a whole-body CT which showed a collection, suspected as abscess, adjacent to the C6-T3 vertebrae, invading the spinal canal, with signs of a pathological fracture in in the T1-2 vertebra, suspected as Pott's disease (Figure 1A).
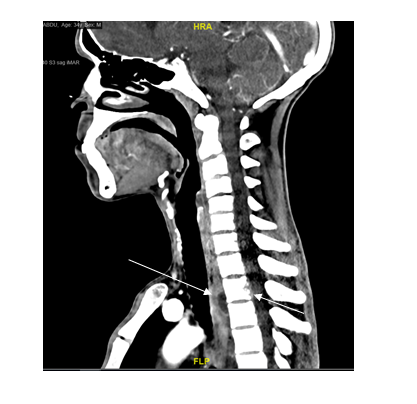
Figure 1a:CT of cervical spine demonstrating a fluid collection adjacent to C6-T3 vertebrae and pathological fractures in T1-2 vertebrae

Figure 1b: Pelvic CT demonstrating two fluid collections in the psoas muscle
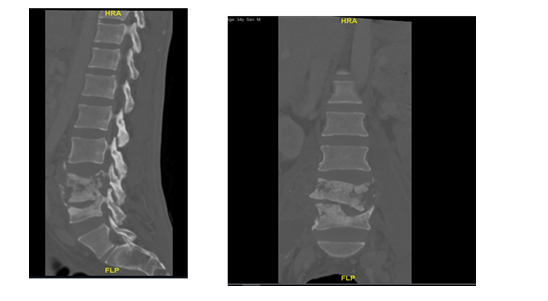
Figure 1c:Lumbar CT in a sagittal and coronal view, demonstrates lumbar vertebrae involvement
Bilateral collections were also demonstrated in the psoas muscles, with invasion and pathological fractures of adjacent vertebrae (Figure 1B, Figure 1C). The patient was totally asymptomatic regarding his COVID-19 infection. The psoas muscle collections were externally drained and microbiological examination of the pus was positive for TB on both PCR and culture. After multidisciplinary consultation, including neurosurgeons and infectious diseases specialists, a conservative (non-surgical) therapeutic plan was elected. The patient was treated with Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol as well as with corticosteroids.
Case number 2
A 32-year-old Eritrean – born male patient, with a past medical history of untreated type 2 diabetes mellitus, presented with one week of cough, shortness of breath and postprandial nausea and vomiting. He denied fever, weight lost, night sweat or hemoptysis. Upon ER admission, a chest x-ray was performed and revealed an infiltrate in the right upper lobe. PCR of SARS-CoV-2 was positive with cycle threshold (Ct) value of 26, and the patient was admitted to a COVID-19 designated ward. Chest CT demonstrated a large consolidation in the right upper lobe, with smaller infiltrates in the right lower lobe and enlarged mediastinal lymph-nodes (Figure 2).
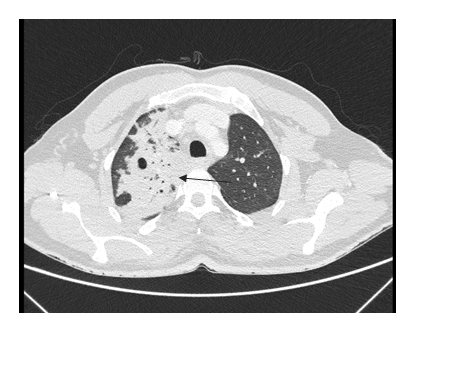
Figure 2:Chest CT demonstrating a large consolidation in the right upper lobe, with smaller infiltrates in the right lower lobe
No evidence of COVID-19 typical imaging findings were found. Induced sputum was preformed and was positive on Ziehl-Neelsen stain and a positive PCR of Mycobacterium Tuberculosis(MTB) was found. Treatment was started with Isoniazid, Rifampicin, Pyrazinamide and Ethambutol. Twenty-one days later, PCR of TB and Ziehl-Neelsen stain in sputum were negative.
Case number 3
A 30-year-old Eritrean – born male with no significant past medical history, was presented with productive cough, abdominal pain accompanied with postprandial nausea and vomiting for the last two weeks. The patient reported reduced appetite and weight loss over the last few weeks. He denied fever, night sweats, hemoptysis or diarrhea.
Upon examination in the ER, chest x-ray demonstrated a small-to-moderate bilateral pleural effusion. PCR for SARS-CoV-2 was positive with cycle threshold (Ct) value of 17, and the patient was admitted to a COVID-19 isolation ward for further evaluation. On admission, chest CT was performed and showed a left loculated pleural effusion within the interlobar fissure, round atelectasis, and a small right pleural effusion with pleural thickening in the posterior aspect of the lung (Figure 3A). No evidence of COVID-19 typical imaging findings was found.

Figure 3a: Chest CT demonstrating a left loculated pleural effusion within the interlobar fissure, round atelectasis, and a small right pleural effusion with pleural thickening in the posterior aspect of the lung.

Figure 3b:Pelvic CT demonstrating involvement of L3-L4 vertebrae and penetration of the spinal canal.
Abdominal - pelvic CT showed ascites with enhancement and thickening of the peritoneal layers, with nodular omental infiltration and necrosis. Spinal damage was also demonstrated, with L3-L4 involvement and penetration of the spinal canal (Figure 3B). A hypodense organized process ("cold abscess") was visible within the psoas muscle as well as inguinal adenopathy. The findings were interpreted as being compatible with Pott’s disease.
Multiple sputum tests returned negative for both MTB PCR and culture, as well as for Ziehl – Neelsen stain. A Pleurocentesis yielded 250ml of exudative fluid. Fluid tests showed an ADA level of 53U/L, with no evidence of empyema, negative bacterial culture and no malignant cells. A peritoneal tap showed serosal fluid with ADA level of 67U/L. Eventually, an excisional biopsy of an inguinal lymph node was performed which was positive for MTB PCR and culture. He started treatment with Isoniazid, Rifampicin, Pyrazinamide and Ethambutol.
Outcome and Follow-Up
In all three patients, a rapid clinical improvement was observed, with no subsequent neurological deficit. All patients were referred for follow up and treatment at a specialized Tuberculosis center after discharge.
Discussion
Notwithstanding the immense impact of the COVID-19 pandemic, TB, one of the most ancient of human infectious diseases, remains a major cause of morbidity and mortality worldwide.
Tuberculosis, one of the classical great masqueraders, may currently challenge the diagnosis of COVID-19, sharing similarities in various aspects. Thus, social factors such as lower socioeconomic condition, overcrowding and diabetes; mode of transmission through airborne droplets; clinical symptoms such as fever, cough, weakness may all overlap between TB and COVID-19,[3]. Currently, relatively little is known regarding the clinical significance of co-infection with these two pathogens, e.g., regarding the possibility of COVID-19 causing reactivation of latent TB or exacerbation of active disease. Similarly, it is hard to estimate to what extent TB may increases the risk of developing severe COVID with pulmonary manifestations such as ARDS and thromboembolism.
In the course of COVID-19, immunopathological damage is mainly attributed to the low lymphocytes count caused by SARS-CoV-2, which initiates an aggressive inflammatory response and tissue damage through increased levels of cytokines and enhanced pulmonary neutrophile infiltration. Theoretically, COVID-19 /TB co-infection might lead to a delay in the development of the cytokine storm typical of severe COVID-19 on the one hand, while on the other hand late-stage T-cell exhaustion may predispose to TB reactivation. Thus, Pathak et al,[4], have reported on a stem cell - mediated defense mechanism activated by COVID-19 which may activate latent TB.
Mousquer et al,[5] have reviewed six studies of patients with COVID-19 /TB co-infection. They suggest that both active and previous history of TB may increase susceptibility to SARS-CoV-2 and worsen the clinical course of COVID-19 infection. A study conducted by Liu et al,[6], also suggested that patients with TB are more susceptible to SARS-Co-2 and to progression to severe COVID-19 disease. On the other hand, Chen H. et al have suggested that COVID-19 might boost the progression and development of TB,[7] while additional recent reviews have asserted that there is no evidence of a direct association between TB and COVID-19 progression [8-10].
In the three herein reported cases, all patients were asymptomatic, and without any typical imaging findings, regarding their COVID-19 infection. Based on the history and clinical manifestations, patients 1 and 3 appear to have developed active extra-pulmonary TB before being infected with COVID-19. In these patients, we assumed COVID-19 may have worsened TB manifestations.Based on Patient 2 history and clinical display, he appeared to develop active pulmonary TB adjacent to COVID-19. In this case we assumed COVID-19 promoted his TB pulmonary disease. Whether the extent of spread of the extra pulmonary mycobacterial disease in these young, otherwise immunocompetent patients may indicate a deleterious immunomodulatory effect of SARS-CoV-2 infection is hard to establish.
According to a recent review by Di Gennaro et al and by WHO report, the impact of COVID-19 pandemic on TB has resulted in a diagnostic delay, reduction in hospitalization, increment of severity of clinical manifestation and TB death [11-12]. However, all three cases reported here occurred among patients born in Eritrea and living in Israel for several years. This population is considered to be at high risk for TB infection and may suffer from difficulties at acquiring medical attention, thus being at risk for delayed diagnosis. Earlier detection of unsuspected tuberculous infection due to COVID-19 related imaging is thus an unexpected positive effect.
Learning Points/Take Home Messages
In conclusion, the current case report demonstrates the association of SARS-CoV-2 with active tuberculous infection, both pulmonary and extra pulmonary, and raises the question of a possible immunomodulatory link between the two processes. On the other hand, the cases draw attention to the possibility of early diagnosis of TB during the COVID-19 pandemic, due to increased hospitalization and investigation of patients with COVID19, particularly in populations in which TB is endemic and access to medical care is limited.
Further research is warranted regarding the immunological and epidemiological interactions between SARS-CoV-2 and Tuberculosis
● Due to increased hospitalization and investigation of patients with COVID19 in Israel, number of early Tb diagnosis cases increased.
● There is an association of SARS-CoV-2 with active tuberculous infection, both pulmonary and extra pulmonary
● SARS-CoV-2 infection may worsen Tb manifestation or prompts Tb pulmonary disease.
● MTB infection did not seem to influence on COVID-19 clinical manifestations.
References
1. Harding E. WHO global progress report on tuberculosis elimination. The Lancet Resp Med. 2020;8(1):19.
2. Esakandari H, Nabi-Afjadi M, Fakkari-Afjadi J, et al. A comprehensive review of COVID-19 characteristics. Biol Procedures Online. 2020;22:1-0.
3. Singh A, Prasad R, Gupta A, et al. Severe acute respiratory syndrome coronavirus-2 and pulmonary tuberculosis: convergence can be fatal. Monaldi Archives Chest Dis. 2020;90(3).
4. Pathak L, Gayan S, Pal B, et al. Coronavirus activates a stem cell-mediated defense mechanism that reactivates dormant tuberculosis: implications in COVID-19 pandemic. BioRxiv. 2020.
5. Mousquer GT, Peres A, Fiegenbaum M. Pathology of TB/COVID-19 Co-Infection: The phantom menace. Tuberculosis. 2020:102020.
6. Liu Y, Bi L, Chen Y, et al. Active or latent tuberculosis increases susceptibility to COVID-19 and disease severity. Medrxiv. 2020.
7. Chen H, Zhang K. Insight into the impact of the COVID-19 epidemic on tuberculosis burden in China. Eur Resp J. 2020;56(3).
8. Gao Y, Liu M, Chen Y, et al. Association between tuberculosis and COVID-19 severity and mortality: a rapid systematic review and meta-analysis. J Med Virol. 2020:10–12. doi: 10.1002/jmv.26311
9. Singh A, Prasad R, Gupta A, et al. Severe acute respiratory syndrome coronavirus-2 and pulmonary tuberculosis: convergence can be fatal. Monaldi Arch Chest Dis. 2020;90 doi: 10.4081/monaldi.2020.1368.
10. Bandyopadhyay A, Palepu S, Bandyopadhyay K, et al. COVID-19 and tuberculosis co-infection: a neglected paradigm. Monaldi Archives for Chest Dis. 2020;90(3).
11. World Health Organization (WHO). Global Tuberculosis Report; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240013131 (accessed on 7 February 2021).
12. Di Gennaro F, Gualano G, Timelli L, et al. Increase in Tuberculosis Diagnostic Delay during First Wave of the COVID-19 Pandemic: Data from an Italian Infectious Disease Referral Hospital. Antibiotics. 2021;10(3):272.
Received: February 02, 2022;
Accepted: February 21, 2022;
Published: February 24, 2022.
To cite this article : Bannon L, Shlesinger O, Kinaany F, et al. The Bright Side of COVID-19 Pandemic Vis-À-Vis Neglected Diseases: Three Asylum Seeker -Patients with TB- COVID19 Co-Infection. European Journal of Respiratory Medicine. 2022; 4(2): 294 - 297. doi: 10.31488/EJRM.129.
© 2022 Bannon L, et al..
